After an informed public that is knowledgeable about the risk factors for oral cancer, the dental community is the first line of defense in early detection of the disease. Including both generalists and specialists, there are over 100,000 dentists in the US, each one seeing between 8 and 15 patients per day. If you include those patients who come to a practice and see someone other than the dentist, such as the hygienist, the number of patient visits is significantly higher. The American Dental Association states that 60% of the US population sees a dentist every year. Just doing “opportunistic” cancer screenings of the existing patient population which visits a dental office every day, would yield tens of thousands of opportunities to catch oral cancer in its early stages. One of our goals is to initiate an effort within the dental community to aggressively screen all of the patients who visit their practices. At the same time, we are launching a public awareness campaign. This campaign is intended to drive public awareness of oral cancer and to instill in the public’s mind the need for an annual screening for this disease. To augment the efforts of professionals, we are launching a “Check Your Mouth” campaign in January 2018 which will encourage people to, between dental visits at home on a monthly basis, do a self-examination of their mouths looking for things which are new, appear abnormal, and are persisting. This will then lead to self-referral to a dental of a medical practitioner for evaluation of the suspect area and definitive diagnosis of what it is. A dedicated website www.checkyourmouth.org has been established that has a simple how-to video on self-screening to get everyone started easily. The idea of self-examination is not new, and in other cancers that lend themselves to this idea such a melanoma and breast cancer, the idea of at-home examinations has had huge benefits. Oral cancer should be impacted the same way once the adoption of the idea has taken place by a large enough segment of the population. One only has to look at the impact of the annual PAP smear, mammogram, and prostate exam, to see how effectively an aware and involved public can contribute to early detection when coupled with a motivated medical community. The dental community needs to assume this same leadership role if oral cancer is to be brought down from its undeserved high ranking as a killer.
Published studies (Horowitz et. al. in two studies ten years apart) show that currently, less than 15-25% of those who visit a dentist regularly report having had an oral cancer screening. Most frequently when it is done it is accomplished by the RDH in the office and not the doctor. RDH’s are qualified to do these screenings and bring suspect areas to the attention of the doctor in the office for further examination and potentially additional diagnostic procedures such as biopsy. This low percentage of patients screened is unfortunate, when you consider that historically, the greatest strides in combating most cancers have come from increased awareness and aggressive campaigns directed at early detection. It is now commonplace to annually get a PAP smear for cervical cancer, a mammogram to check for breast cancer, or PSA and digital rectal exams for prostate cancer. These screening efforts have been possible as a result of the increased public awareness of the value of catching cancers in their earliest stages of development, combined with effective technologies for conducting the examinations. Oral cancer is no different. Actually, it is potentially easier to obtain public compliance for oral cancer screenings, since unlike many other cancer screening procedures, there is no invasive technique necessary to look for it, no discomfort or pain involved, and it is very inexpensive to have your mouth examined for the early signs of disease. Education of the public regarding the risk factors which lead to oral cancer, and the development of public awareness, are primary responsibilities of the dental community.
It is important that both private individuals, and members of the dental community, realize that a visit to the dentist is no longer about a filling, a crown, or a postponable cleaning, but is actually a matter of life and death. Dental examinations, when properly done and which include a screening for oral cancer, will save lives. If you are a dental professional, we encourage you to become a member of the foundation, and partner with us in this effort to increase the number of annual screenings that are being done. Please check within the dental area of our website where the issue from a practice management perspective is discussed, and where you can find resources to assist you in the incorporation of a comprehensive cancer screening program in your practice.
Discovery and diagnosis
Historically, it has been difficult to determine which abnormal tissues in the mouth are worthy of concern. The fact is, the average person routinely has conditions existing in their mouths that mimic the appearance of pre-cancerous changes and very early cancers of the soft tissues. One study determined that the average dentist sees 3-5 patients a day who exhibit soft tissue abnormalities, most of which are benign in nature. Even the simplest things, such as apthous ulcers, herpes simplex, herpes labialis, the wound left by accidentally biting the inside of your cheek, or sore spots from a poorly fitting prosthetic appliance or denture, all at first examination, share similarities with dangerous lesions. Some of these conditions cause physical discomfort, others are painless. The question is which ones deserve action, and which ones bear watching and waiting?
There has been a tendency to watch these areas over an extended period to determine if they are dangerous or not. Unfortunately, this philosophy leads to a situation in which a dangerous lesion may continue to prosper and grow into a later stage, hard to cure cancer. Any sore, discoloration, induration, prominent tissue, irritation, hoarseness, which does not resolve within a two week period on its own, with or without treatment, should be considered suspect and worthy of further examination or referral. Besides a routine visit to the dental office for regular examinations, it is the patient’s responsibility to be aware of changes in their oral environment. When these changes occur, they need to be brought to the attention of a qualified dental professional for examination. The dental professional needs to be current in the knowledge base necessary to make a proper diagnosis, and be competent in the proper screening procedures to identify oral cancer.
How to know if you have had a proper oral cancer screening
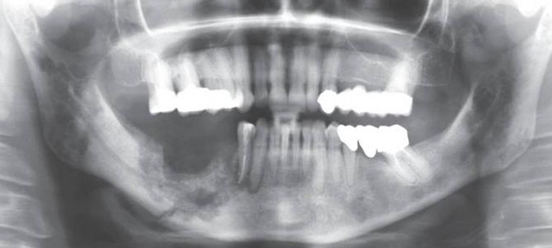
There are two separate issues, discovery, and diagnosis. Discovery is the result of a thorough visual and manual examination. A protocol for a comprehensive oral cancer screening appears elsewhere in this section of the web site. It includes a systematic visual examination of all the soft tissues of the mouth, including the manual extension of the tongue to examine its base, a bimanual palpation of the floor of the mouth, and a digital examination of the borders of the tongue, and the lymph nodes surrounding the oral cavity and in the neck. New diagnostic aids, including lights, dyes, and other techniques are beginning to appear in the marketplace. While potentially making the discovery process more effective, it is still possible to do a comprehensive examination through a proper visual and tactile process without adjunctive devices.
Click here for additional information on screening
Once suspect tissues have been detected, the only way a definitive diagnosis of oral cancer may be made is through biopsy. While some salivary diagnostic tests and biologic marker tests have become available on the dental market, no major pathology organizations have endorsed them, and they have arrived for sale through a laboratory standards protocol which avoids FDA oversight and approval to market. Until their efficacy has been endorsed by a major pathology organization or the FDA, the foundation will not be a supporter of these tests, and we do not consider them adequate alternatives to conventional laboratory histopathology. Given a large number of tissue abnormalities a dentist sees every day, it is not logical, nor practical, that each one of these be biopsied. The first question which may help in the determination of which abnormality bears closer examination, is how long has the suspect condition been present? Any condition that has existed for 14 days or more without resolution should be considered suspect and worthy of further diagnostic procedures or referral. Certainly, it is common knowledge that two of the most prevalent lesions that mimic oral cancer are herpes simplex ulceration, and aphthous ulcerations, each resolve on their own in approximately 10-14 days. Perhaps that sentence should be underlined, since one of the most common primary diagnoses received with referred patients to a major university cancer pathology department is “an atypical herpetic/aphthous lesion” These all too frequently turn out to be squamous cell carcinomas, which have been under observation…. for several months.
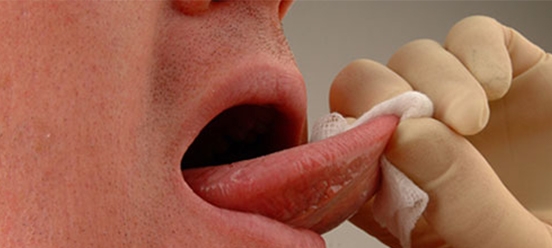
A detailed description of brush cytology, and the oral brush biopsy.
Note that this brush cytology collection system is not designed to provide the kind of information, specifically cellular architecture, that would be obtained through a punch or incisional biopsy. But it will provide an answer to the question of whether malignancy exists or not, through a quick, minimally invasive, and inexpensive procedure. Should positive results be returned through this system, the brush biopsy must be followed by a conventional biopsy procedure for confirmation. The argument for the brush biopsy is that it eliminates the waiting and watching of a suspicious lesion, while it develops from a highly treatable and curable, early-stage localized cancer, into a life-threatening late stage malignancy. Positive identification of oral cancers at the earliest stages, result in the best prognosis for long-term survivability.
Creating awareness, discovery through screening, diagnosis, or referral for diagnosis, and when appropriate referral to medicine for treatment. When it comes to oral cancer and saving lives, these are the primary responsibilities of the dental community. This is dentistry’s cancer. The most important step in reducing the death rate from oral cancer is early discovery. No group has a better opportunity to have an impact than members of the dental community.
Start a dialog with your patients today. Even if talking about cancer with them is difficult, there are mechanisms around this.